For over a decade I worked, as a Clinical Psychologist in a service treating people who had suffered trauma. I clocked just under ten thousand hours of clinical contact with people who had been through the worst situations imaginable. One thing I learned during that time is that trauma often occurs to us as an interruption.
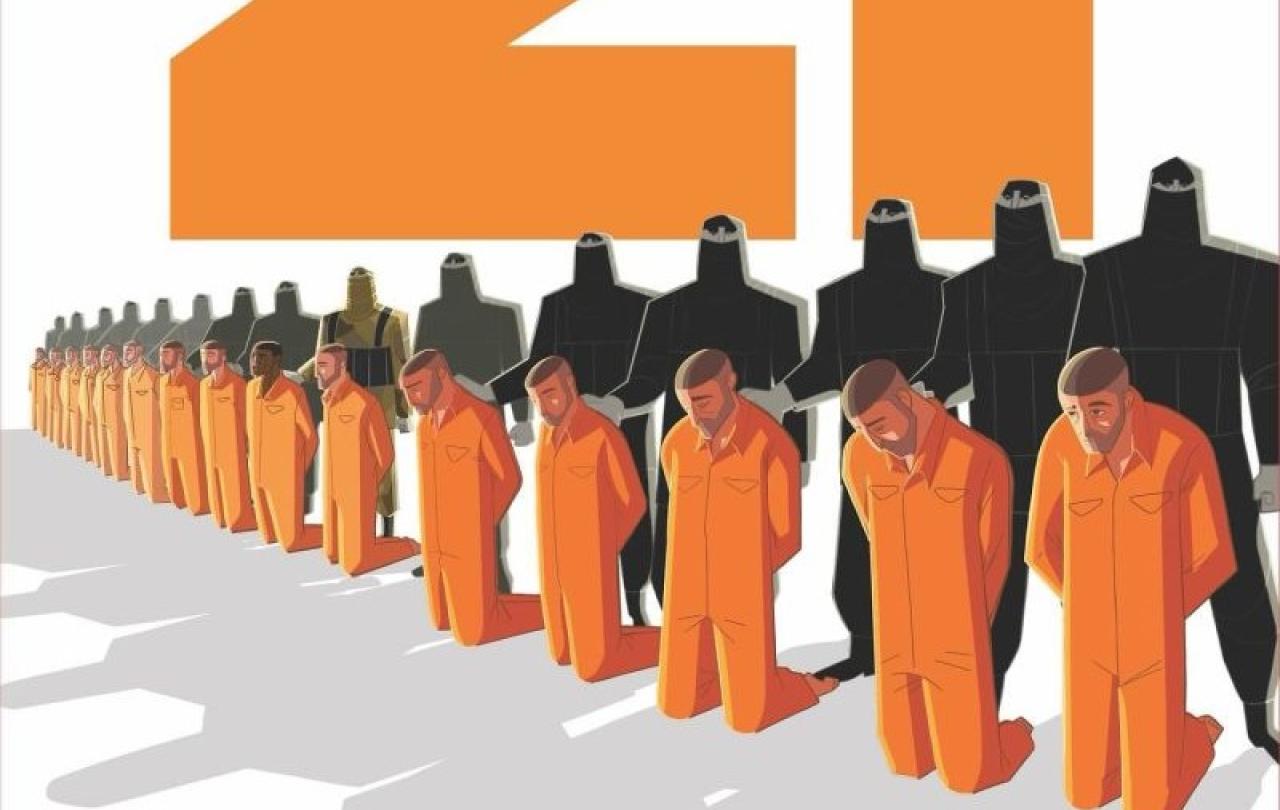
Most of us live our lives to some script, a set of assumptions of how we think things should be, our expectations of what is about to happen next - and trauma shatters those assumptions. Over and over again, people who had been through trauma told me how their view of the world had been violated. The narrative that defined their life, the story they thought they were in, changed genre unexpectedly. The romcom became a horror movie; the adventure became a hideous farce. The story called walking home at night turned into another one called being mugged. Driving to the supermarket became, having a crash. A day out at the beach, became delivering CPR. All of them illustrate how trauma sends an earthquake through our view of what we thought our lives were and, if we survive, leaves us in the rubble picking up the pieces.
In one fell swoop it gave an insight into why it is that trauma occurs to us, not just as an event or a set of events, but as an interruption to our whole sense of reality.
Back in the early days of researching AI systems one study illustrated the catastrophic effect that even the mildest contradiction of our expectations can have on our entire view of reality.
In the quaint old days, when Chat GPT was a nightmare for a future generation, an expert system was developed with one simple aim in mind: to identify birds. Such a simple task. The specifications of various species of animal were entered and, by applying a broad array of criteria, the system would indicate whether the said species was a bird (or not). But not all its criteria were accurate. One of the rules of thumb the system developed was: ‘all birds fly’. Which worked fine until it was required to categorize a penguin. In the first attempt it followed its own rules and concluded that penguins were not birds. But when forced by the programmers to categorize a penguin as a bird, the system went into meltdown attempting to reconcile the contradiction with its own criteria. To resolve the anomaly of the penguin being flightless and yet still being a bird, it concluded that no birds could fly. In one fell swoop it gave an insight into why it is that trauma occurs to us, not just as an event or a set of events, but as an interruption to our whole sense of reality.
The nightmares, the flashbacks, the apprehension, irritation and sense of foreboding, the numbing and the terror. All of these are an attempt to make sense of a world that no longer makes sense. Of course, it would be heartless to suggest that the agony of trauma is little more than a glitch in our information processing. Reducing it to a bug in our programming would conveniently trivialise the horrors that can befall human beings. I have no desire to sanitise or diminish the horrors that can haunt us, but trauma is at least this - a hiatus, a shock, an interruption.
The agony that intensifies our fears, depressions and compulsions is often the torturous comparison between who we thought we were and who we have become.
It is not just trauma that interrupts us. Life specialises in throwing wildcards and anomalies into our path. Just when everything seems to be going swimmingly, when we seem to know what we are doing, when the future seems mapped out before us, the unexpected and the unwelcome occurs. The best way to make God laugh, goes the saying, is to hand Him our five-year plan. I’m not sure I have ever spoken to anyone with insight into their own psychological distress who doesn’t to some extent experience their pain as an interruption. The agony that intensifies our fears, depressions and compulsions is often the torturous comparison between who we thought we were and who we have become. Our imaginary ideal self, the person we thought we would be, waltzes away into a future of freedom, light and joy, and leaves us behind in doubt and uncertainty.
Mental Health Week could in some ways be viewed as an acknowledgement of the interruptions in life. I can only imagine what has interrupted you. I can only hazard a guess at what it is or was that derailed the smooth trajectory of your predicted life. Was it bereavement or aging, sickness or betrayal, disappointment or assault, redundancy or financial ruin? Whatever it was, it may not be reversible. This is one of the reasons for the burgeoning of mindfulness practices in mental health treatment. We don’t just need a technology of change to help us get better, we equally need a technology of acceptance to be able to live with what we cannot change.
I’ve lost the ability to firmly believe that the future can be planned out, that the straight line into the next few years cannot be shattered without warning at any moment.
For me, the lockdown was an interruption from which I have never really recovered. I hesitate to say this because I worry I might be the only person who feels this way. I know it’s all supposed to be over. We’re back to work and acting like the world is rational and predictable again. But the great reset just doesn’t work for me. My mind is ready to go, but my heart just hasn’t got the memo. I’ve lost the ability to firmly believe that the future can be planned out, that the straight line into the next few years cannot be shattered without warning at any moment. There is a hesitancy in all my plans, an uncertainty in my ambitions. The solid arrow of time is dotted, if not broken. Experts in trauma call it the sense of a foreshortened future. The disruption of our capacity to self-transcend, to bridge ourselves towards the person we may become. Our once lucid image of a better self flickers and grows dim, no longer compelling or believable.
And if that’s not confession enough, I have another one. One that makes me sound like a rehab resident in a young adult drama. In the midst of the lockdown craziness, I was forced to slowly and reluctantly uncover a gift. Like a treasure buried in a field, or a priceless pearl concealed among the worthless tat of a car boot sale. Something so crashingly obvious and cringeworthily twee that I can hardly bear to put it in writing. Many of my plans and ambitions were imaginary, just plain illusion. I was no happier achieving them than I was pursuing them. But I started to glimpse, that if I could overcome the grief of losing them, I would be better off without them. If I could put words to it, I would say that I came to a deeper appreciation of grace – iit’s not a bad thing just to be. We can be so busy trying to become something that we fail to notice that we were before we even began. This has now become a daily contemplative practice for me. I call it being present to The Presence in the present. Somehow, I came to a deep inner settlement that I no longer needed to work to justify my existence, but could work out of a present moment in which my existence was already justified. I came to accept acceptance.