Statistically speaking, autistic people are far more likely to die by suicide than non-autistic people. They are also, statistically speaking, far more likely to die by physician assisted suicide than non-autistic people, in countries where this is allowed.
For example, in a study of 927 people who sought physician assisted suicide in the Netherlands (where this is legal) 39 of them were autistic. That’s about four per cent, but the prevalence of diagnosed autism in the Netherlands is only one to two per cent. The researchers go on to note that 21 per cent of these 39 people cite autism or intellectual disability as the “sole cause of suffering” that had prompted them to request assistance to die.
I don’t like speaking statistically. For a start, 21 per cent of 39 people is 8.19 people, which raises obvious questions. A little digging reveals that what the researchers mean really is eight people. Eight people with eight unique stories that include an account of autistic suffering so intense that they asked for help to end their lives.
But we do not have those stories, not really. Included in the report are carefully anonymised excerpts from the physicians’ notes, and this is the nearest that we can get.
‘The patient suffered from his inability to participate in society [ … ] [He] was not able to live among people, because he was easily overstimulated. This made him isolated’ (2019 (22), male, 70s, ASD)
‘The patient had felt unhappy since childhood and was persistently bullied because he was just a bit different from others [ … ] [He] longed for social contacts but was unable to connect with others. This reinforced his sense of loneliness. The consequences of his autism were unbearable for him [ … ] The prospect of having to live on in this way for years was an abomination to him and he could not bear it’ (2021 (26), male, 20s, ASD)
The debate about legalising physician assisted suicide in the UK is ongoing, and the British Medical Association have provided a helpful guidance document which sets out the main arguments, both for and against, without making a recommendation either way. In the document, they observe that the reasons people ask for assisted suicide are predominantly personal and social, not clinical, and also that “laws send social messages.” I agree that laws do that, and I also think that those seeking assisted suicide send social messages too.
For example, even just from these two tiny excerpts, I hear that a life worth living is one where people can participate in society and have social contacts, even if they are a “just a bit different from others.” It would be good to hear more. It would be good to sit down over a cup of coffee with each of these two men and ask them all my questions about their lived wisdom when it comes to autism.
I could ask “2019 (22), male, 70s, ASD”:
What causes the overstimulation - are there places where you don’t feel that?
Can we create more such places for autistic people to socialise?
And I could ask “2021 (26), male, 20s, ASD”:
What makes you feel different?
What kind of social contacts and connections do you think that you are looking for?
But of course, I can’t do that, because these two men have been assisted to die.
The word ‘welcome’ is striking to me here. What does it mean to welcome someone, not to merely include or tolerate, but to really welcome someone.
When approached for comment, autistic theologian Claire Williams said:
‘There is something of a personal and social tragedy reflected in these cases. If we understand that much of the difficulty that autistic people suffer is caused by society – as per the neurodiversity paradigm – then it is the case that these two nameless men were failed by society. They felt that their lives could not find a place in an unwelcoming world. It is, of course, their choice to end their lives but I do also think that God chose to start their lives and finds them to be infinitely valuable. They were both made in God’s image and reflect something of it. That they felt there isn’t a place for them that is suitable is a tragedy because society should do better to welcome them.’
The word ‘welcome’ is striking to me here. What does it mean to welcome someone, not to merely include or tolerate, but to really welcome someone, even if they seem ‘a little bit different from others’? Dr Léon van Ommen, another theologian who writes about autism, suggests that it is a matter of making oneself and one’s resources fully available to that person, to the point where they feel that you belong to them. This is not to promote relationships with unhealthy power dynamics, but to highlight that when a person feels truly welcomed by another, they feel the opposite of owing a debt or being a burden – they feel they are of value, that you would be lacking something without them.
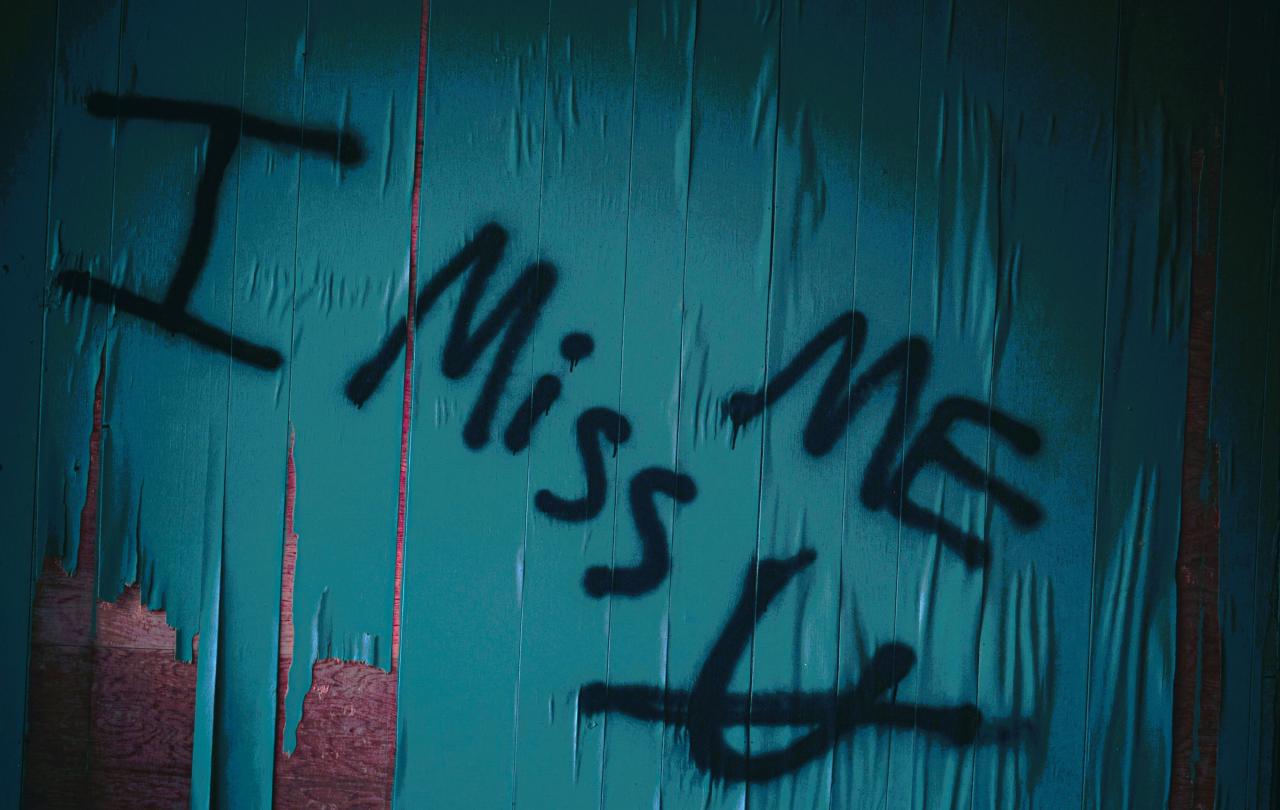
I feel we are lacking something without you, “2019 (22), male, 70s, ASD”. And I feel we are lacking something without you, “2021 (26), male, 20s, ASD”. Not to forget the 37 others who are a little like you. We can pause to reflect on the social messages that you have sent, what you are teaching all of us about what it means to live a “good” life. But I am sorry that you have all died now and we cannot hear more.
Whether people in the UK should be able to choose physician assisted suicide, I, personally, am not yet sure. Like the BMA, I see and respect the very good arguments both for and against. But eight people have chosen physician assisted suicide due to autism or intellectual disability, and when it comes to the social messages that sends, I feel compelled to sit down and listen.